India Toolkit: Services & Supply
- Home
- Help and Support
- Close
- Toolkits
- Global Toolkit
- AYSRH Toolkit
- Hub Toolkits
- Core High-Impact Practices
- Gender Essentials Mini Course
- Close
- Resource Collection
- Community of Practice
- Coaching
- Log In/Register
- My Profile
- English
Fixed Day Static Services/Family Planning Day Approach to Expand Access To Quality Family Planning Services
 Purpose: This tool provides specific guidance on expanding access of quality Family Planning (FP) services at the doorstep of the most vulnerable populations, including urban poor. For the same, it coaches on thow to implement Fixed Day Static (FDS) Services/ Family Planning Day (FPD) /Antral diwas for offering the family planning basket of choice, including Long-Acting Reversible Contraception (LARC)/spacing methods at urban primary health centers (UPHCs), other higher order public facilities and accredited private sector health facilities.
Purpose: This tool provides specific guidance on expanding access of quality Family Planning (FP) services at the doorstep of the most vulnerable populations, including urban poor. For the same, it coaches on thow to implement Fixed Day Static (FDS) Services/ Family Planning Day (FPD) /Antral diwas for offering the family planning basket of choice, including Long-Acting Reversible Contraception (LARC)/spacing methods at urban primary health centers (UPHCs), other higher order public facilities and accredited private sector health facilities.
Audience:
- Additional Director / Joint Director (AD/JD)
- General Manager (GM) FP and Urban
- Chief Medical Officers (CMO)/Additional Chief Medical Officer (ACMO)
- Chief Medical Superintendents (CMS)
- Divisional Urban Health Consultant (DUHC)/District Program Manager (DPM)/Urban Health Coordinator (UHC)
- City Community Process Manager (CCPM)/FPLMIS Manager
- District Quality Assurance Committee (DQAC)
- Medical Officer In-Charge/Medical Officers (MOICs/MOs)/Persons In-Charge of Private Facilities/Staff nurses
- NGO/Health Partners
Background: The FDS/ FPD approach has been seen to increase access and availability of quality FP services. It helps the government maximize the use of its limited resources, including human resources, and increase the provision of services to a large number of beneficiaries. It is a collaborative effort wherein trained human resources, equipment, commodities and supplies at the facility are made available on a pre-announced day and time, known to the community.
The FDS/ FPD approach is consistent with the government strategy. It is organized on a regular basis on the same day to offer a range of FP methods or a specific method such as No-Scalpel Vasectomy (NSV), Female Sterilization (FST), Intra Uterine Contraceptive Device (IUCD) or Injectable. The FDS/ FPD can be organized in government facilities as well as in accredited private facilities. When organized in the private sector, the service burden on the government health facilities is reduced, thus providing the underserved greater access to FP methods and services.
How FDS/FPD/Antral Diwas increases satisfaction and trust of users in health facilities
- Individuals receive FP services they have come for, unless they are screened out on medical grounds
- High quality services with counselling and appropriate follow-up are provided
- The service schedule is widely publicized and is easy to remember
- Waiting time is minimal
- Increases access and provide assured quality FP services on a fixed day
Evidence of Effectiveness
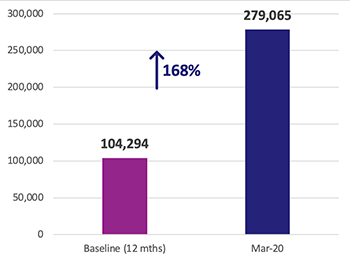
Figure 1: Increase in annual clients accessing FP services across TCI cities in India.
The government officials of Uttar Pradesh, Madhya Pradesh and Odisha implemented FDS/FPD approach with the coaching and mentoring support of The Challenge Initiative (TCI) India. Across 31 intervention cities of these three states, the FDS/FPD approach helped the government to maximize its use of limited human resources and increase the provision of FP in 503 urban primary health center (UPHCs). The experience revealed that when FDS/ FPD for FP were regularly organized in a facility, they enhanced the quality and utilization of routine FP services in that facility.
TCI India conducted two rounds of population-based surveys, which found that the modern contraceptive prevalence rate among currently married women (ages 15 to 49) in poor areas of cities increased significantly from 49.8% in Round 1 (September 2018) to 53.7% in Round 2 (September 2019). Furthermore, UPHC Health Management Information System (HMIS) (NHM, HMIS, 2019) data show that the TCI India program contributed a 168% increase in annual FP client volume as of March 2020 (compared with baseline), or 175,671 more clients accessing FP care (Figure 1). The UPHC proportion of FP clients is around 67% of the total annual FP client volume at the city level.

Figure 2: Estimated acceptors in family planning method in TCI, India,
Sep 2017-Feb 2020 UPHCs only
HMIS trends also show a rapid increase of short-acting reversible methods, including injectable contraceptives, and an increase in IUCD use. Figure 2 represents the increase in annual FP client volume. To prevent overestimation of short-term methods, HMIS data have been adjusted using standard couple-year protection, which is the total estimated protection provided by contraceptives in a one-year period. To account for seasonal variations, the data represent a 12-month average for short-acting methods and rolling sums for long-term and permanent methods. An increase in the trend therefore means that the latest month outperforms the same month from the last year.
With the support of TCI India, we rolled out Fixed Day Static (FDS) in a staggered manner across 52 UPHCs and 8 UCHCs. This resulted in electrifying increase in overall FP users, motivating government to expand FDS to all rural and urban PHCs across all 75 districts, in the form of ‘Antral Diwas.”
– Dr. Narendra Agarwal, Former Chief Medical Officer, Lucknow, Uttar Pradesh
Guidance for Implementing FDS/FPD/Antral Diwas
1. Making family planning data visible by estimating the unmet need based on available data
To amplify how health systems must focus and prioritise FP, data from population-level studies, HMIS and project health information systems must be triangulated and discussed at both city and state level FP monitoring meetings. FP uptake data disaggregated by age/ parity and method choice is critical for a city to plan its FDS/FPD strategy to reach women with unmet need for FP.
2. Determining the schedule of FDS/FPD for district hospitals, UPHCs, urban community health centers (CHCs) and accredited private health facilities
The state government should issue a directive to districts to initiate FDS/FPD in all types of facilities. The CMO can designate a day for FDS/FPD. A medical/facility in-charge can also request permission to conduct FDS.
In accordance mobilize community and ensure facility readiness. Further specific guidance to organize FDS/FPD is listed here:
- The CMO should issue a directive to facilities to share their FDS/ FPD calendar, after which a schedule can be drawn. (Refer to: Government FDS calendar format).
- The schedule submitted should include the proposed dates, the range of FP services to be provided and the FDS/ FPD medical team consisting of a doctor, an anaesthetist (if applicable), paramedical staff, a lab technician, a counsellor, a ward boy and a sweeper that would be made available. The CMO would then approve the schedule and budget as required.
- CMO can leverage public private interface meeting (PPIA) to coach accredited private providers to organize FDS/ FPD to expand choice of providers for the vulnerable population.
- The FDS/ FPD calendar should be widely circulated through community of practice/WhatsApp group among health staff and front line workers like Accredited Social Health Activists (ASHA) and Anganwadi Workers (AWW).
- Community mobilizers and other community members should be informed about the FDS/ FPD schedule through door to door visits by ASHAs, by Auxiliary Nurse Midwife (ANMs) in urban health nutrition day (UHND) sessions, through handbills, newspaper inserts and other communication mechanisms for publicizing the information.
3. Ensuring facility readiness for FDS/FPD/Antral Diwas
The MOIC, CMS/ facility-in-charge of accredited private facilities should ensure constitution of the FDS/ FPD team and assign responsibilities to ensure that commodities, supplies, equipment, human resource, requisite reporting forms and Information, Education and Communication (IEC) materials are available on the given day.
- Review of facility readiness by MOICs/MOs, CMS and private providers along with other quality improvement (QI) team members a day before the FDS/FPD. Electricity, water supply, clean wash room, infection prevention and proper plan for complication management are also important requirements for quality services. The checklist for UPHC (site readiness format) and higher order facilities (checklist for preparedness of site during FDS for sterilization procedure) can be used to assess and ensure facility readiness.
- A duty roster should be created by the facility-in-charge for all essential staff i.e. medical and non-medical, including anaesthetists (in case of district hospital and accredited private facilities), staff nurses, lab technicians, counsellors, drivers, sweepers etc.
Where a facility does not have trained medical/ paramedic staff required for providing any particular FP services, such as lack of doctors trained in IUCD, injectable contraceptive (Antara) NSV and the facility-in-charge should seek help and approval from the CMOs to depute qualified staff from another facility or to hire a private sector doctor for FDS/ FPD. Further, CMO should drive training of service providers on all appropriate basket of choice methods. - The CMS of the government facilities and the facility-in-charge of accredited private facilities should ensure that the wage loss compensation is paid to the sterilization clients and incentives are paid to the motivators (wherever applicable)
District quality assurance committee / members should visit the facility a day or two before the day of FDS/FPD. - The counselor or the designated staff member should establish a separate registration counter for FP clients on the day of the FDS/ FPD and client information should be recorded in a register.
- The counsellor/staff nurse should offer pre-service counseling to clients (Refer to: Final draft of handbook on FP for counselors and paramedics, Chapter nos. 2 to 6) and respond to their queries with the help of IEC materials (Refer to: UHI’s method-specific IEC materials)
- From here, the client should be sent to the Out Patient Department (OPD), where a designated/ empaneled doctor should examine and screen the woman or man prior to the procedure/ service. The doctor may also refer the client for any further diagnostic tests.
- Based on the screening, the client should be offered the FP method of his/ her choice and in case the client is not fit for a particular FP method, then appropriate counseling should be done regarding the other available suitable methods.
- From here, the client should be sent to the Out Patient Department (OPD), where a designated/ empaneled doctor should examine and screen the woman or man prior to the procedure/ service. The doctor may also refer the client for any further diagnostic tests.
- Based on the screening, the client should be offered the FP method of his/ her choice and in case the client is not fit for a particular FP method, then appropriate counseling should be done regarding the other available suitable methods.
- All documentation should be completed. In the case of sterilization, the consent form, the medical case record checklist and the client card should be filled out and the client card copy should be given to the client (Refer to: Government consent form & other checklists for sterilization).
- The accredited private facilities should utilize the government approved client records and reporting forms including the consent forms.
- The counsellor/staff nurse should provide post-procedure counseling to all those who have received the service. This should include information about the necessary follow-up, possible side-effects and early warning signs which require immediate medical attention by a provider (Refer to: Final draft of handbook on FP for counselors and paramedics, Chapter no. 13).
- Condoms (in cases of NSV) and medicines for follow-up care should be given along with the client card before the client leaves the hospital.
- The facility-in-charge can arrange for pick-up and drop for sterilization clients by arranging government ambulance services such as 108.

4. Mobilization of the community to participate in the FDS/FPD/Antral Diwas
- Coaching and mentoring of ASHAs is an essential step to strengthen demand generation activities for FDS/FPD. (Refer to TCI India tool- Enabling urban ASHAs) and for this ASHAs should to be coached on the following:
- Providing informed choice counseling and referrals
- Devising an “FP due list” of eligible couples based on UHIR and 2BY2 matrix data
- Using FP job aids and communication materials for counseling eligible couples and responding their questions about FP methods
- Linking the community with FDS.
- Publicize FDS/FPD through Auxiliary Nurse Midwife (ANMs), Accredited Social Health Activists (ASHA), Anganwadi Workers (AWW), Mahila Arogya Samiti (MAS), OPD, wall poster at facility/UHND, field staff of NGOs and local community of practice/WhatsApp group of ASHAs.
- ASHAs, other developmental partners and NGOs should publicize FDS/ FPD services through different IEC materials like wall posters and handbills, which carry information about dates and venues of FDS/ FPD to mobilize the clients.
- The FDS/ FPD date can be publicized by stamping it on the OPD registration forms in government facilities as well as in private and NGO facilities.
- To publicize the FDS/ FPD, local media can be briefed by the CMO.
Roles and Responsibilities
General Manager FP and Urban
- Ensure timely procurement of FP commodities from the state to strengthen supply chain management
- Review FP data of urban facilities -UPHCs, higher order facilities and private facilities
- Issue guidance to all the districts/cities to refer this tool as one of the guidance documents for implementation of FDS/FPD for spacing method at UPHCs and for all methods at other public and accredited private sector health
AD/JD
- Review FP data of the cities of the division to take decisions and provide guidance
- Replicate best practices of performing cities with other cities to strengthen FP data of the division
CMO/ACMO
- Send a directive to the persons in-charge of all the facilities and accredited private facilities to obtain facility-wise FDS/ FPD schedule and to approve and allocate resources
- Encourage all accredited private facilities to organize FDS/ FPD
- Proactively plan and organize FDS/ FPD in the district
- Ensure that empaneled providers are available for conducting FDS/ FPD
- Monitor quality and outputs of each facility
- Review FDS data by facilities in district level review meetings
CMOS/MoIC/Facility in-Charge (In case of private facilities)
Coach to ensure the following:
- Devising FDS/ FPD calendar, establishing FDS/ FPD teams and facility readiness
- Informed choice and method-specific counseling is done as per guidelines
- Clients are appropriately screened. In case, they are not eligible for their preferred method, clients should be counseled about other appropriate contraceptive alternatives
- Methods are provided with appropriate quality of care including recommended infection prevention practices
- Monitor the quality of FDS/FPD services and ensure correct reporting.
- Wage loss compensation for sterilization clients
- Minimize waiting time for clients at the facility on the day of FDS/ FPD
Nodal Officer- Urban Health and FP/DUHC/DPM/UHC
- Lead in planning and organizing FDS/ FPD in the district
- Manage the FDS/ FPD operations including team deployment and logistics
- Coordinate and oversee all quality parameters and work as an interface between district leadership and facilities
- Ensure methods are provided with appropriate quality of care including recommended infection prevention practices
- Ensure a smooth supply of commodities and supplies
- Monitor FDS/ FPD for quality and ensure data validation and reliability
- Ensure client verification for accredited private facilities.
Staff nurse/Facility counselor
- Develop the FDS/ FPD calendar and establishing FDS/ FPD teams
- Supervise facility readiness prior to FDS/FPD
- Provide informed choice and method-specific counseling to clients
- Ensure that clients are appropriately screened
- In case the client is not eligible for their preferred method, they should be counseled about other appropriate contraceptive alternatives
- Ensure that methods are provided with appropriate quality of care including recommended infection prevention practices
- Monitor the quality of FDS/ FPD services and ensure correct reporting
- Ensure wage loss compensation for clients to be sterilized
- Minimize client waiting time at the facility on the day of FDS/ FPD
- Do post-procedure follow-up of clients
ANMs/NGO
Coach community health workers (ASHA, MAS, AWW, NGO outreach workers) on the following:
- Generate awareness and mobilize clients for FP through home visits and group meetings
- Prepare potential client list before each FDS/ FPD
- Use IEC materials to provide information to men, women and community leaders about FP and specific contraceptive methods
- Use handbills to provide information on FDS/ FPD schedules and availability of services
- Accompany clients to the facilities to help them access services
- Share client’s feedback with the facility-in-charge on services
- Support post-procedure follow-up of clients
Monitoring FDS/FPD/Antral Diwas
FDS can be monitored by including FDS/ FPD as a regular agenda item for discussion in the Facility level QI Team, DQAC meeting, District Health Society (DHS) meeting, and monthly meeting of MOIC convened by the CMO. The following indicators should be reviewed:
- Number of FDS/ FPD planned as compared to the number of FDS/ FPD held
- Number of FP clients served through FDS/ FPD, and their method-mix distribution
- Percentage of FP clients served through FDS/ FPD vis-a-vis total FP clients served, by method and by month
- Client-provider ratio for sterilization (to ensure that client safety and quality of care is not compromised)
Further, spot checks by the CMO/ACMO-Nodal/DUHC/UHC and by in-charge of facility should be undertaken to ensure attention to quality parameters and resolution of bottle-necks. Monitoring the reasons for which women are screened out or service provision is postponed, particularly for sterilization, can provide important information on quality of care and provider-driven barriers to services. This information can be obtained by noting the reasons for screening out/ postponement in the client register.
Data Quality Assurance
Although there is a tendency to collect and report service provision data from FDS/ FPD together with the data from routine service days, separate record-keeping for a certain period of time is recommended for monitoring and validation.
Cost Elements
The elements required for FDS/ FPD are mentioned below along with their Program Implementation Plan (PIP) codes for easy reference. They may be covered under existing budget line items, but if not, they should be incorporated through the PIP. Any additional support can also be sought from the flexi-pool. The table below is indicative and illustrates the manner in which cost elements are provided in a government PIP, thus giving guidance to the audience on where to look for elements related to a particular task, such as implementing FDS/ FPD services.
Sl. No. |
FMR Code |
Budget Head |
| 42 | RCH 6 | Sterilization – Female |
| 43 | RCH 6 | Sterilization – Male |
| 44 | RCH 6 | IUCD Insertion (PPIUCD and PAIUCD) |
| 45 | RCH 6 | ANTARA |
| 46 | RCH 6 | MPV(Mission Parivar Vikas) |
| 47 | RCH 6 | Family Planning Indemnity Scheme |
| 48 | RCH 6 | FPLMIS |
| 50 | RCH 6 | IEC |
| 51 | RCH 6 | State Specific Innovation (Private Sector – Hausala Sajheedari) |
Source: NHM PIP Guideline 2022-2024
Sustainability
Sustainability of FDS/FPD can be achieved through the following measures:
- Select and set one day in a week when assured high-quality FP will be provided at facility. Equip facility with trained human resources, equipment, and supplies for FDS/FPD days. To strengthen demand, coach ASHAs on prioritizing client, preparing FP due list, publicizing FDS days in community and mobilizing clients on FDS/FPD. Ensuring that financial resources required for FDS/ FPD are included in the annual PIP.
- Establish a routine schedule of implementation through an order by the CMO and institutionalize monitoring in monthly meetings.
- Make a specific staff member accountable for FDS/ FPD (for example, a doctor/ matron/ senior nursing staff of a District Womens Hospital (DWH) or the in-charge of a private accredited facility) at each facility. By making quality FP services more frequently available at a facility, FDS/ FPD serves as a first step towards providing comprehensive FP services on a regular basis. FDS/ FPD at the DWH and other accredited private facilities have become a regular practice where a broad range of FP services are provided. Still, the need is to continuously publicize the event in poverty clusters and other slum areas to create demand.
- Ensure that providers have skills and knowledge to provide all methods (as it decreases the need for contracting-in providers on special days and facilitates availability of all methods on a regular basis). Ensure periodic refresher training of service providers on method techniques.
- For sustaining FDS/ FPD in private accredited facilities, constant follow-up should be done with private providers by the CMO or his designated nodal officer to motivate them, build their capacity, provide them timely reimbursements and support them in generating demand for FP services on the FDS/ FPD days.
TCI APP USERS PLEASE NOTE
You will only receive CERTIFICATES by email – when earning a score above 80% – and will not be able to view or print a certificate PDF from the TCI app.
Test Your Knowledge
Earn a Certificate
Quiz Summary
0 of 5 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Results
0 of 5 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 5
1. Question
FDS increases satisfaction and trust in the health facilities through:
CorrectIncorrect -
Question 2 of 5
2. Question
Essential staff for FDS includes:
CorrectIncorrect -
Question 3 of 5
3. Question
Sustainability of FDS can be achieved through:
CorrectIncorrect -
Question 4 of 5
4. Question
How useful did you find the information and/or tools presented on this page? Please write your response in the box below using one of the following phrases: Very useful, Useful, Somewhat useful, Not useful.
Feel free to comment on why you made that choice.
-
This response will be awarded full points automatically, but it can be reviewed and adjusted after submission.
Grading can be reviewed and adjusted.Grading can be reviewed and adjusted. -
-
Question 5 of 5
5. Question
How do you intend to use the information reviewed and/or tools that you accessed?
-
This response will be awarded full points automatically, but it can be reviewed and adjusted after submission.
Grading can be reviewed and adjusted.Grading can be reviewed and adjusted. -
Service Delivery Approaches
Infographics
Available Resources
- Annexure 6 checklist for preparedness of site during FDS for sterilization procedure
- Exit interview for client on FDS (refer Standards & Quality Assurance in Sterilization Services, Annexure 19, Page 95
- Facility Audit Checklist (Refer to Standards & Quality Assurance in Sterilization Services, Annexure 6, Page 72)
- Final Draft Handbook on FP for counsellors and paramedics, Chapter No. 2 to 6
- Final Draft Handbook on FP for Counsellors and Paramedics, Chapter No. 13
- Government consent form & other checklists for sterilization
- Govt. FDS Calendar Format
- Pregnancy screening checklist (GOI / PSI / USAID)
- Reference manual for Female Sterilization (GOI guidelines)
- Reference manual on Male Sterilizations (GOI Guidelines)
- Standards and quality assurance in comprehensive family planning services in private facilities through “Fixed Day Static” Approach (PSI-EAQ Project)
- Standards & Quality Assurance in Sterilization Services (GOI, Nov. 2014)
- UHI / Govt. Approved IEC Resource Materials (Handbills, posters etc)
- TCIHC site readiness format
- NHM PIP Guideline for a particular financial year
- TCI Enabling urban ASHAs
- 2BY2 Matrix tool
- WHO IBP- Fixed-Day Static Approach: Informed Choice and Family Planning for Urban Poor in India














