Women in their first year after childbirth have the highest unmet need for family planning (FP); more than two-thirds of these women want to delay their next birth but are not using any method. Although postpartum women frequently visit health facilities, FP methods are not often offered to, or taken up by them.
One way to increase access to FP services is through integration with maternal and child health (MCH) services, such as antenatal care, delivery, postnatal and child immunization visits.
Limited research has been completed as to the most effective ways to integrate these services for the greatest impact. This study explored the potential role of the integration of FP services into MCH services to improve access to postpartum FP use in urban Senegal, by:
- Examining women’s exposure to FP information and services at the time of delivery and at child immunization appointments, and
- Determining whether these points of integration were associated with greater use of postpartum FP.
The authors used data collected for the Measurement, Learning & Evaluation baseline survey in 2011 from the urban sites of Dakar, Guédiawaye, Pikine, Mbao, Mbour and Kaolack. Data came from two cohorts: 1) for the facility-based interviews, women who visited high volume public and private facilities for FP and reproductive health services; and 2) for the household survey, women currently in union, who had had a birth in the last two years and who were not pregnant at the time of the interview.
Study Results
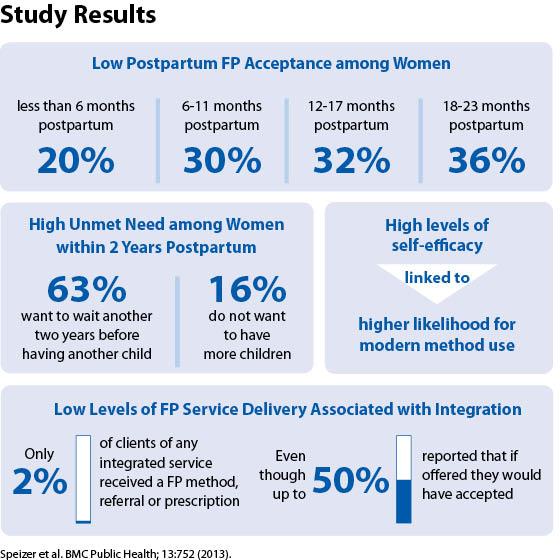
Study results revealed that there were low levels of acceptance of FP in postpartum women while there is a high level of unmet need among women with two years postpartum.
- Use of modern FP varies by birth history and postpartum duration. The shorter the postpartum period, the less likely women will use a modern contraceptive. FP acceptance was highest (36%) among women who had given birth in the past 18 to 23 months, compared to 20% for women who were less than six months postpartum and 32% for women between 12 and 17 months postpartum.
- There is high unmet need for FP methods among postpartum women. Although only 36% of women were using a modern method, 63% of women who were within two years postpartum indicated that they wanted to wait another two years or more before having another child. Another 16% did not want to have more children.
- Women with high self-efficacy were significantly more likely to be using a modern FP method. Levels of self-efficacy were determined based on eight questions asked of women, including their confidence starting a conversation on FP, obtaining a FP method, and using a method even if her partner did not want to.
- While the majority of clients knew that FP information or methods were available in the facilities they were visiting, only 2% of clients of any of the services received a FP method, referral or prescription during their visit.

Among postpartum women, those within 18 to 23 months postpartum are the most likely to be using a modern family planning (FP) method. Women who have had a child in the last six months are the least likely to use a modern FP method (19.5%); those between 18 and 23 months postpartum are most likely (35.9%).
The study found that labor & delivery and immunization services are missed opportunities for the integration of FP services, as the majority of postpartum women (those who delivered in a facility and those who sought child immunization services) did not receive FP information or counseling and were not using any FP method at the time of these visits. Between two-fifths and one-half of women reported that, if they had been offered a FP method, they would have accepted it. However, only 26% of women who sought postnatal care received information about FP. Only 5% of women attending immunization clinics and 9% of women at the time of delivery or who were receiving post-abortion care got information about FP.
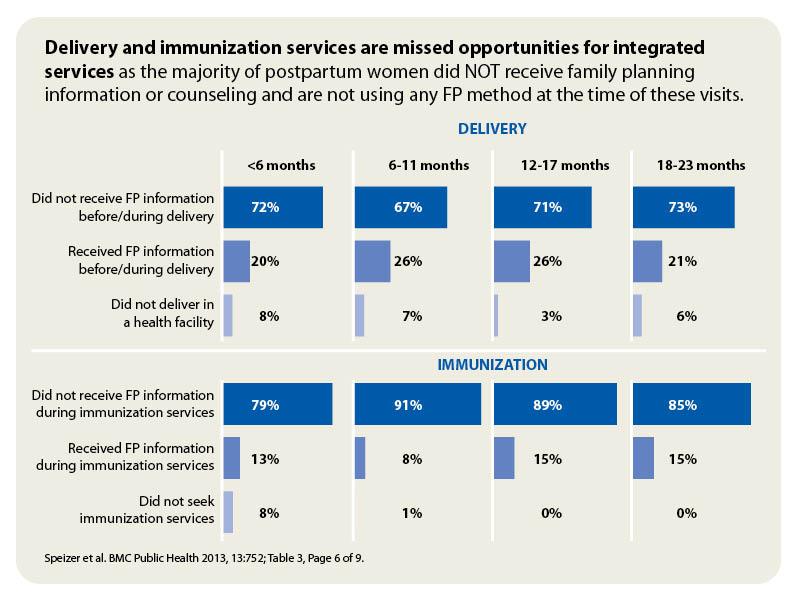
The majority of postpartum women did not receive family planning information or counseling and are not using any FP method at the time of these visits.
The study revealed that women who delivered at a health facility and did not receive FP information were less likely to use FP than those who had received information. Similarly, women who had not gone to health facilities for child immunization visits were significantly less likely to use a modern FP method than those women who had gone to a clinic for these services.
Results show that integrating FP into delivery and postpartum services in high volume settings is associated with greater FP use.
Programmatic Implications

Using multivariate regression odds ratios, this graph shows that women who delivered at health facilities and received information regarding FP were more likely to be using a modern FP method at the time of the survey when compared with women who had not.
The study results indicate that the integration of FP into MCH services provides an opportunity to reach women with unmet need for spacing or limiting births. Results show that integrating FP into delivery and postpartum services in high volume settings is associated with greater FP use. The analysis provides evidence of the need to focus resources on integration as a means to improve access to FP services since many postnatal and immunization clients would have accepted a FP method if offered at the time of a visit. To fill this gap in postpartum FP services, several interventions should be undertaken, including training providers in service provision, counseling, and outreach services.
This story was originally written by the Measurement, Learning & Evaluation Project, which evaluated the Urban Reproductive Health Initiatives (UHRIs) in Kenya, Senegal, Nigeria and India. The Challenge Initiative is charged with expanding access to the proven solutions and successes developed under the UHRIs.


